Understanding Your Costs
The first thing to know is that a covered service or benefit, in most cases, is not free to you. There are costs that come with most care. Knowing the costs that come with your care can help you feel better about visiting your PCP or other provider.
Your Schedule of Benefits and Summary of Benefits and Coverage
The member materials you received when you enrolled included your Schedule of Benefits and Summary of Benefits and Coverage. They show the costs for covered services on your plan and examples of how those costs are applied in different settings. You can also find these documents in your My CareSource® portal account under Documents, and on CareSource.com/marketplace under Plan Documents.
Schedule of Benefits Example
Summary of Benefits and Coverage Example
My CareSource
If you haven’t set up a My CareSource member portal account yet, please do! My CareSource has your private CareSource information and so much more. Go to MyCareSource.com to sign up. Have your CareSource ID card ready. You will need your Member ID number. Your account not only has your Schedule of Benefits and Summary of Benefits and Coverage, but it shows all of your Explanations of Benefits and claims too. You can also see a graph that shows how much you have paid toward your annual deductible and maximum out-of-pocket amounts.
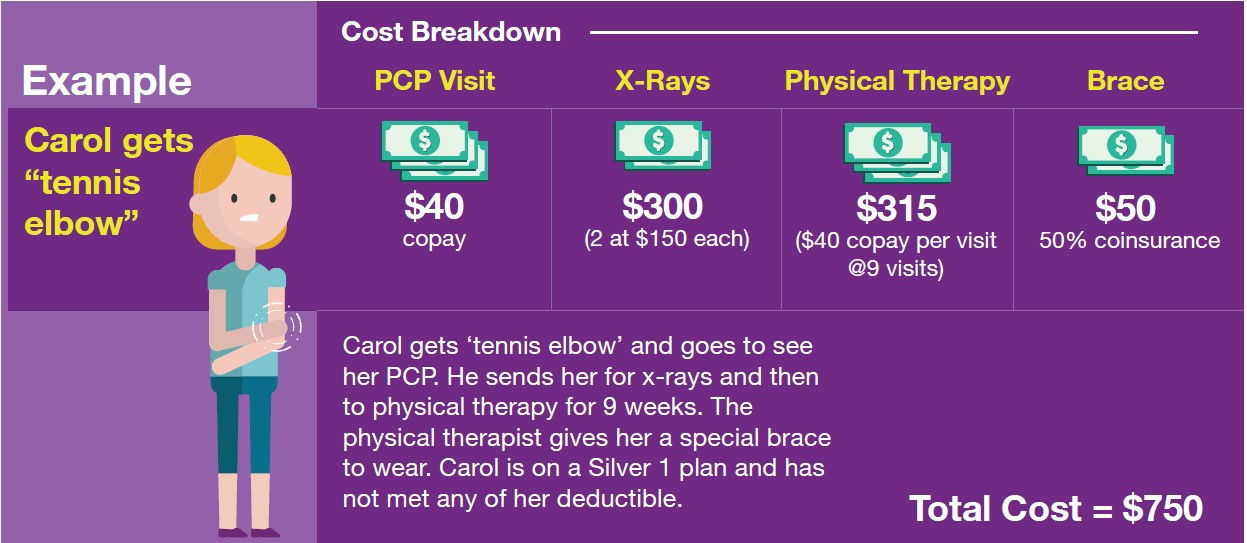
Cost Shares
Cost shares are the amounts you pay for care and services. They define how you and CareSource will share the cost of your care. Cost shares are either a copay or coinsurance, based on your plan and the type of service you get. For example, most office visits have a copay, while an x-ray or other test might have a coinsurance.
A copay is a flat dollar amount and is paid by you whether or not your deductible has been met. A coinsurance is a percentage of the cost of a service. It is normally paid after your deductible has been met.
Your costs can change based on where you get care or the type of provider you use. Generally, your costs will be lower for care from your PCP, higher if you go to an urgent care, and even higher in the emergency room.
Some preventive care services are provided at no charge. That means that CareSource pays the full cost of these services. Learn more about preventive care guidelines by age here.
Annual Deductible
Your annual deductible is the specific amount of money you must pay out-of-pocket before CareSource begins to share the cost with you. This does not include copays or care that is no charge to you. You can see these listed on your Summary of Benefits and Coverage or Schedule of Benefits shown on the plan Documents page.
Cost Example: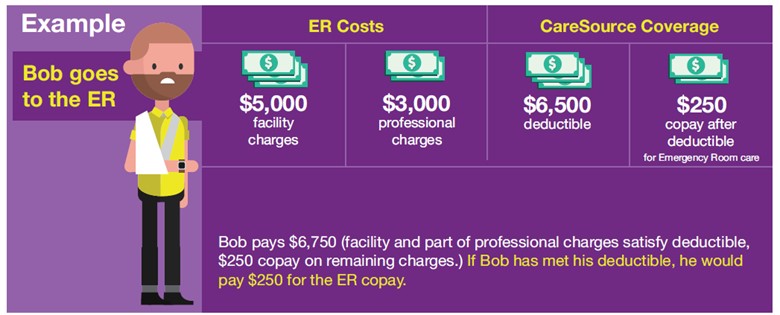
Maximum Out of Pocket (MOOP)
Your Maximum Out-of-Pocket amount is also shown on your Schedule of Benefits and Summary of Benefits and Coverage. It is the most you have to spend on covered care or services during any benefit year. The MOOP does not include any copays, non-covered or excluded care and services.
Billed Amount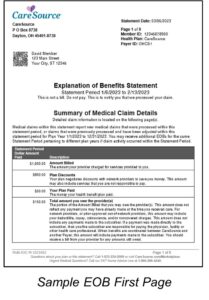
This is the amount that your provider charges for the services they provide. This may not always be the amount you pay, but it can influence the amount you have to pay. If you go to a provider who charges more for services than others, the portion you have to pay may be higher if the services you get are subject to deductible or coinsurance. You will see this on your Explanation of Benefits (EOB). Your EOB will also show you the amount you owe. You will get an EOB in the mail from us after you visit a provider or fill a prescription.
We negotiate rates with our network providers to keep costs low, while making sure that you get high quality care and respect for your rights as a member. That is why we do not cover services from out-of-network providers except in emergency, urgent or other rare instances.
If you think you need care from an out-of-network provider, please call Member Services at 1-833-230-2099 (TTY: 711) Monday through Friday, 7 a.m. to 7 p.m. Eastern Time for help.
Get Help When You Need It
Call Member Services or Care Management if you need help. Member Services can help answer questions about your EOB or claims. If you need more in-depth help understanding your benefits and what your coverage pays for, a Care Manager will be happy to help you. Our Care Management department is open Monday through Friday 8 a.m. to 5 p.m. Eastern Time at 1-833-230-2037.